 |
 |
 |
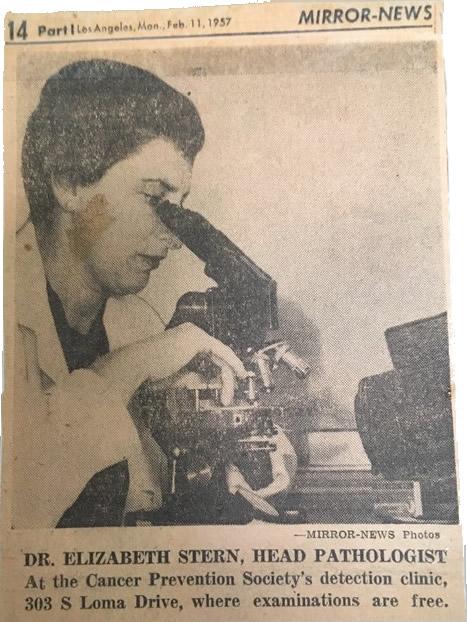 |
Defining the Earliest Stages of Cervical Cancer
How do doctors know if a patient
is at risk for disease? In the case of cervical cancer,
physicians have the Pap test which screens patients for
cervical cancer. As a part of this test, pathologists
examine cervical cells under a microscope to check for
abnormal cell shape and size. Tissues from this test can
be used to identify precancerous stages of cervical
disease often before patients show symptoms. The ability
to monitor patients for early signs of cervical cancer
is fundamental to diagnosis and treatment, and has
helped improve rates of patient survival and remission.
Her research formed a cornerstone of cervical cancer
diagnosis and treatment planning. In order to fully
appreciate what Dr. Stern accomplished over her
decades-long career, it is important to understand the
role of cytopathology in cervical cancer studies as it
developed from the 1950s into the twenty first century.
***
Today, if abnormal cells are found from the Pap test,
they can easily be defined as pre-cancerous or
cancerous, and further ranked by stage depending on
results of additional biopsies. These pre-cancerous
stages are termed dysplasia, or cervical intraepithelial
neoplasia (CIN), and are included in textbooks or
journal articles on cervical cancer diagnosis. Although
dysplasia itself is not cancer, these small changes in
cell structure are a strong indicator of abnormal tissue
growth that may lead to cancer if left unchecked. Dr.
Stern’s findings were a major advance in the field of
cervical cancer and helped establish the field of
cytopathology. For the first time, physicians had a more
effective cancer screening method to identify patients
at various stages and initiate treatment in a timely
manner.
(see Figure 1).
Dr. Stern realized that the Pap test presented a unique
opportunity to fully characterize all stages of cervical
cancer development. Cervical cancer is usually a slowly
developing disease, and even in the 1950s it was known
that cervical cancer can take decades to fully develop
into a tumor and cause symptoms. By only focusing on
cervical cancer stages that have already formed tumors,
physicians were missing a wealth of potentially relevant
data that could help them diagnose patients at even
earlier stages.
Dr. Stern and other researchers had noted the small
changes in cervical cell shape and size in patients who
did not display any symptoms and did not have treatable
cancer. But Dr. Stern hypothesized that these cellular
abnormalities could be useful markers in at-risk
patients.
Many physicians were still skeptical of using cellular
changes as a method to diagnose cancer, much less
characterize pre-cancerous stages not causing physical
symptoms. Dr. Stern’s ideas about dysplasia and the
potential applications of cytopathology were considered
radical at the time.
Dr. Stern’s career spanned more than three decades, and
during this time her lab conducted multiple long-term
studies in Los Angeles County. Thousands of patients
were examined from different racial and socioeconomic
backgrounds for varying periods of time, up to 10 years
in some cases [1-7]. The central conclusion of this
exhaustive work confirmed her hypothesis. Patients that
developed cervical cancer first displayed pre-cancerous
cellular abnormalities (dysplasia) in Pap tests. These
studies are also inextricably linked to her work on the
birth control pill, public health, and improvement of
the Pap test which are detailed on the other pages of
this site.
***
Although Dr. Stern published dozens of papers on this
topic, she faced significant pushback in the early years
of her work. Nevertheless, by the time she passed away
in 1980, dysplasia was increasingly recognized as a
warning sign of cervical cancer. Furthermore,
cytopathology had become a widely accepted area of
research and today is a standard method for cancer
diagnosis.
Figure 1 outlines the impact of her
work on how the Pap test is used to identify patients
with pre-cancerous cells in modern medicine.
REFERENCES:
1. Stern E. Epidemiology of dysplasia. Obstet Gynecol
Surv. 1969;24(7 Pt 2):711-23.
PubMed PMID: 5212425.
2. Stern E. Cytological screening for cervical cancer;
comparative findings in a 6 year survey of a well
population. Cancer. 1958;11(1):122-6.
PubMed PMID: 13500307.
3. Stern E. Rate, stage, and patient age in cervical
cancer. An analysis of age specific discovery rates for
atypical hyperplasia, in situ cancer, and invasive
cancer in a well population. Cancer. 1959;12:933-7.
PubMed PMID: 13834430.
4. Stern E. Cytohistopathology of cervical cancer.
Cancer Res. 1973;33(6):1368-78.
PubMed PMID: 4718680.
5. Stern E, et al. A cytological scale for cervical
carcinogenesis. Cancer Res. 1974;34(9):2358-61.
PubMed PMID: 4843536.
6. Stern E, Neely PM. Dysplasia of the Uterine Cervix.
Incidence of Regression, Recurrence, and Cancer. Cancer.
1964;17:508-12.
PubMed PMID: 14136534.
7. Stern E, Neely PM. Carcinoma and Dysplasia of the
Cervix: A Comparison of Rates for New and Returning
Populations. Acta Cytol. 1963;7:357-61.
PubMed PMID: 14074943. |
|
|
|
|
|