 |
 |
 |
 |
The Link Between Original, High-Estrogen Birth Control
Pills and Cervical Cancer
The birth control pill was first
approved in the United States for contraceptive use in
1960. Today, it is a
leading form of contraception in
the U.S. and is generally considered a safe and
effective method for preventing pregnancy. The pill can
also be used to manage acne,
menstrual disorders, and to help treat pelvic pain. In
addition, there are several health benefits to taking
the pill, such as
decreased risk of ovarian and
endometrial cancer.
Birth control pills prescribed today are very different
than those prescribed in the 1960s and
are not even on the market now.
***
The first birth control pill,
Enovid, was a pharmaceutical
goldmine for G.D. Searle. Other companies soon followed.
By 1965 roughly 6.5 million women in the U.S. were
taking an oral contraceptive.
Enovid was developed using laboratory-produced versions
of two essential reproductive hormones, estrogen and
progestin, to prevent ovulation. Ovulation results in
the release of an egg cell, the female reproductive
cell. If there is no egg cell present, then pregnancy
will not occur. Today’s oral contraceptives
work in a similar manner. Despite
their similarity, the original birth control pill is
quite different from the ones prescribed today. One of
the major differences is the amount of hormones in each
pill.
Enovid contained approximately 10 mg of progestin and
0.15 mg of estrogen. In contrast, today’s oral
contraceptives contain 10 to 100 times more hormones.
Enovid contained what are now considered dangerously
high doses of progestin and estrogen. If scientists and
physicians had followed modern clinical trial protocols,
Enovid never would have been given FDA approval. Enovid
was tested in the late 1950s, before safety and
effectiveness of drugs were considered as separate
factors in drug development. The clinical trials for
Enovid had largely taken place in
Puerto Rico, and high doses of
progestin and estrogen were used to make sure women did
not become pregnant.
None of the women that completed the clinical trials
became pregnant. However, the local physician managing
patients for the study reported that many women
displayed serious side effects, including dizziness,
nausea, vomiting, and severe stomach pain. As a result,
nearly a quarter of patients dropped out of the trial
during the first year, and she strongly suggested the 10
mg progestin dose be reduced.
Unfortunately, these side effects were deemed to be
“imaginary” and largely ignored, a common theme in the
treatment of women by the male-dominated medical
establishment at the time. In addition, the researchers
leading the trials in the U.S. (Dr. Gregory Pincus, Dr.
John Rock, and others) did not want to restart the
entire testing process by testing lower doses, as this
would require additional time and money. Due to the
successful outcome of the drug regarding pregnancy, the
study was pushed forward, and by 1960 the drug was
approved in the United States for contraception.
The lack of robust and transparent clinical testing had
major downstream impacts on the women taking the pill.
Physicians weren’t aware of the risks and neither were
their patients. Synthetic hormones were relatively new
in the pharmaceutical world at the time, so physicians
did not have experience with these medications. In
addition, there were no product pamphlets with drug
warnings or papers to sign when picking up a
prescription as there are today.
As early as 1962, new reports of blood clotting had been
linked to Enovid and reported to the FDA . Many women
also experienced nausea, dizziness, and vomiting,
although these were typically dismissed as psychological
problems [1].
By 1970, mounting frustration, activism and
epidemiological evidence led to Senate hearings on the
safety of the birth control pill. These hearings
prompted the FDA to order that all contraceptive pills
include a product insert detailing potential side
effects, a major improvement for women’s health.
These hearings weren’t sufficient to remove the high
dose Enovid pills from the market. Although birth
control pills suffered a short-term loss in sales after
the hearing,
within a year they had fully
rebounded. By 1970 women had other options, many of
which used lower doses of hormones. The
FDA recommended prescribing these
lower dose pills. But the10 mg Enovid pill was still on
the market and many physicians
continued to prescribe it due to
brand loyalty and the assumption that it was safe.
***
The link between heightened hormone levels and
reproductive cancer was well established by 1970, but
not completely understood. Dr. Stern and colleagues had
published multiple studies using rats, in which loss of
hormones seemed to inhibit tumor development [2-4]. They
also studied the impact of birth control pills on cancer
in rats and found that the Enovid-treated rats developed
cancer more slowly [3, 5]. However, reports from other
labs came to the opposite conclusion, making it
difficult to arrive at a consensus (discussed in [3]).
Further, it was impossible to make accurate predictions
about human cancer risk from rat studies.
Throughout the 1970s, more clinical and epidemiological
research was performed regarding the impacts of
high-dose birth control pills. There were links to
breast, cervical, and endometrial cancer, although these
were challenging to study. Cancer may take several
decades to develop, and the majority of women involved
in these studies had been on the pill for less than ten
years. There were very few non-biopsy, noninvasive,
tests at the time to detect early-stage cancer. Doctors
were relying on symptomatic or visible tumors in order
to diagnose cancer in these studies. This led to
conflicting results in highly respected journals and
confusion in the medical field [6, 7].
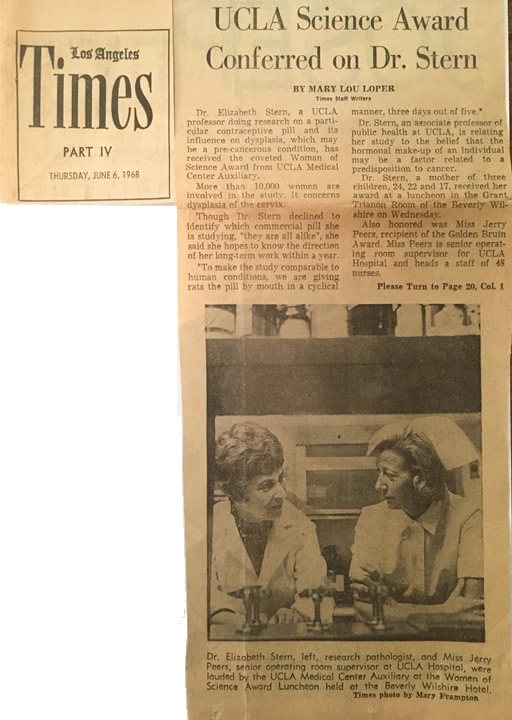
At this time, Dr. Stern had published her groundbreaking
work on how abnormalities in cervical cell shape and
size, dysplasia, were early warning signs of cervical
cancer development. These changes could be detected in
women using the Pap test and confirmed with additional
biopsy studies [8-13]. Dr. Stern reasoned that long-term
monitoring of women with dysplasia, who also were taking
birth control pills, could be useful in determining the
association between the pill and cervical cancer.
Dr. Stern and her colleagues developed a rigorous study
plan [14]. From the more than 11,000 women that came to
the Los Angeles Country Family Planning Clinic between
1967 and 1971, they identified 6,000 patients that had
never taken birth control pills, and enrolled interested
patients into four groups:
1: Pill users that had dysplasia at the outset of the
study by Pap test.
2: Pill users with normal cervical tissue by Pap test.
3: Non-users that had dysplasia at the outset of study
by Pap test.
4: Non-users with normal cervical tissue by Pap test
They examined patients every six months by Pap test for
up to seven years of follow-up study. At each collection
interval, samples were ranked on a 100-point scale
established by Dr. Stern in 1974 [2], in which 0 to 28
is normal, 29 to 62 is dysplasia, and 63 and up is
cancer. They found that women with dysplasia that
started the pill were six times more likely to develop
cervical cancer as opposed to those not on the birth
control pill (Group 3). This difference only became
apparent when analyzing data from six years or more,
suggesting that longer-term studies were crucial to
determine the impact of the high dose birth control
pills on cancer.
These findings were published in Science in 1977 [14]
and made big newspaper headlines, including the
Washington Post. As this article
points out, Dr. Stern’s study didn’t use the high dose
Enovid pill. Nevertheless, this study was important in
further linking hormonal changes to cervical cancer and
supported additional long-term studies on the safety of
oral contraceptives.
Follow-up work, with larger sample
sizes, demonstrated that lower dose birth control pills
were safe, effective and actually helped prevent many
types of cancer, similar to the results Dr. Stern had
first reported in her rat studies. In contrast, long
term use of high-dose pills continued to be linked to
breast and cervical cancer
although these results varied,
underscoring the complicated nature of clinical
research.
Yet higher dose birth control pills, including 10 mg
Enovid, still accounted for nearly 50% of annual sales
as late as 1983. Finally, in 1988,
G.D. Searle and other high-dose pill manufacturers
announced that they would no longer be producing these
drugs at the
urging of the FDA.
Although this research was not Dr. Stern’s main focus,
this work had a significant impact. She brought
attention to negative long-term consequences that were
not fully investigated prior to the drug’s release in
the 1960s. This work also brought to the forefront the
necessity of tissue screening for early-stage cervical
cancer diagnosis and monitoring.
Today’s birth control pills contain significantly lower
doses of hormones and their safety is well-established.
Footnotes:
Women also have more options with progestin-only
pills, low-dose pills, monophasic vs. multiphasic,
extended cycle pills (women only get a period 4 times
per year) as well as non-pill options like the IUD.
Read more here.
The development of the original birth control pill and
subsequent clinical trials were largely run by Harvard
scientist Dr. Gregory Pincus and physician Dr. John Rock
with support from reproductive rights activist Margaret
Sanger and philanthropist/activist Katherine McCormick.
Read more here.
Most of the funding of these studies came from
individual donors such as Katherine McCormick rather
than major pharmaceutical companies.
Newspaper Articles and Reviews:
PBS has several articles on this topic, including a
timeline, details on the
side effects of Enovid, the
clinical trials
performed in Puerto Rico, history
on the involvement of
G.D. Searle, and a review of the
1970 Senate hearings.
An historical perspective on the release of the birth
control pill in the U.S. and the U.K. was written by
Drs. Suzanne White Junod and Lara Marks.
Read it here.
Another article on the controversial aspects of the
development of Enovid, including the Puerto Rican
clinical trials, can be found in the Harvard Crimson.
Read it here.
A review of the people involved in the development of
the birth control pill including Dr. Gregory Pincus, Dr.
John Rock, Margaret Sanger, and Katharine McCormick can
be found
here.
A review from the US Department of Health and Human
Services, Office on Women’s Health: 30 Achievements in
Women’s Health in 30 Years (1984-2014) can be found
here.
References:
1. Liao PV, Dollin J. Half a century of the oral
contraceptive pill: historical review and view to the
future. Can Fam Physician. 2012;58(12):e757-60. PubMed
PMID: 23242907.
2. Stern E, Mickey MR. Neural mechanism in induction of
dioestrus and tumour in the androgen sterile rat.
Nature. 1967;216(5111):185-7. PubMed PMID: 6069882.
3. Stern E, et al. Neuroendocrine factors in
experimental carcinogenesis. Ann N Y Acad Sci.
1969;164(2):494-508. PubMed PMID: 5260542.
4. Stern E, et al. Tumorigenesis in the androgen-sterile
rat: reciprocal incidence of carcinogen induced-mammary
gland and ovarian tumors. Rass Neurol Veg.
1967;21(1):99-117. PubMed PMID: 5617808.
5. Stern E, Mickey MR. Effects of a cyclic steroid
contraceptive regimen on mammary gland tumor induction
in rats. Br J Cancer. 1969;23(2):391-400. PubMed PMID:
5788048.
6. Brinton LA, et al. Long-term use of oral
contraceptives and risk of invasive cervical cancer. Int
J Cancer. 1986;38(3):339-44. PubMed PMID: 3744592.
7. Khoo SK. Cancer risks and the contraceptive pill.
What is the evidence after nearly 25 years of use? Med J
Aust. 1986;144(4):185-90. PubMed PMID: 3511357.
8. Stern E. Epidemiology of dysplasia. Obstet Gynecol
Surv. 1969;24(7 Pt 2):711-23. PubMed PMID: 5212425.
9. Stern E. Cytological screening for cervical cancer;
comparative findings in a 6 year survey of a well
population. Cancer. 1958;11(1):122-6. PubMed PMID:
13500307.
10. Stern E. Cytohistopathology of cervical cancer.
Cancer Res. 1973;33(6):1368-78. PubMed PMID: 4718680.
11. Stern E, et al. A cytological scale for cervical
carcinogenesis. Cancer Res. 1974;34(9):2358-61. PubMed
PMID: 4843536.
12. Stern E, Neely PM. Dysplasia of the Uterine Cervix.
Incidence of Regression, Recurrence, and Cancer. Cancer.
1964;17:508-12. PubMed PMID: 14136534.
13. Stern E, Neely PM. Carcinoma and Dysplasia of the
Cervix: A Comparison of Rates for New and Returning
Populations. Acta Cytol. 1963;7:357-61. PubMed PMID:
14074943.
14. Stern E, et al. Steroid contraceptive use and
cervical dysplasia: increased risk of progression.
Science. 1977;196(4297):1460-2. PubMed PMID: 867043. |
|
|
|
|
|
|